Home / Health / Health Systems Miss Community Care by Focusing Inward
Health Systems Miss Community Care by Focusing Inward
5 Feb
Summary
- Health systems prioritize 'systemness,' potentially overlooking community partnerships.
- Community health workers improve patient trust and education, especially for diverse groups.
- Health literacy gaps require innovative community-based support systems.

Large U.S. health systems are increasingly focusing on internal integration, or 'systemness,' to enhance patient experience and retention against digital competitors. This strategy, however, may inadvertently sideline crucial community partnerships, according to health system and tech leaders. A recent webinar highlighted how overemphasis on internal consolidation can obscure the value of external collaborations. Experts noted that while technology aids patient engagement, trusted community resources are vital for addressing significant health literacy gaps.
Endeavor Health in Illinois exemplifies successful community engagement by integrating community health workers. These individuals enhance trust and communication, particularly with Spanish-speaking or culturally distinct patient groups. By investing in a Community Investment Fund, Endeavor supports local organizations, such as food banks, to provide specific dietary options for patients with conditions like high blood pressure or diabetes. This approach meets patients in familiar environments where they already trust local partners.
Sutter Health in California reports that a third of its adult patients have low health literacy, making complex medical information difficult to comprehend. Community health resources are seen as advantageous, but health systems must adapt their patient communications for better understanding. Similarly, OURA's Chief Medical Officer noted that simplifying navigation within complex health systems is crucial, as initial barriers can prevent patient engagement. Mobile and AI tools can assist, but ensuring accessibility and trust remains paramount for individuals needing critical care.
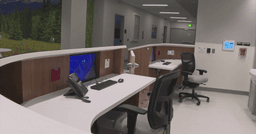
Cleveland Clinic's diabetes initiatives, led by Dr. Kevin Pantalone, benefit from virtual visits and AI scribes. These tools enhance patient interaction by allowing physicians more meaningful engagement during appointments, rather than focusing solely on documentation. This technology supports a more personalized patient relationship. Leaders advocate for health systems to strategically augment care with digital tools while leveraging existing, trusted community institutions for services they excel at, echoing the sentiment that local experience matters most to patients.