Home / Health / Medicare AI Denies Claims: Seniors Face New Barriers
Medicare AI Denies Claims: Seniors Face New Barriers
2 Dec, 2025
Summary
- Six states introduce AI for Medicare coverage decisions starting January 1.
- Critics fear AI will increase claim denials due to financial incentives.
- The AI program aims to reduce fraud and waste in traditional Medicare.
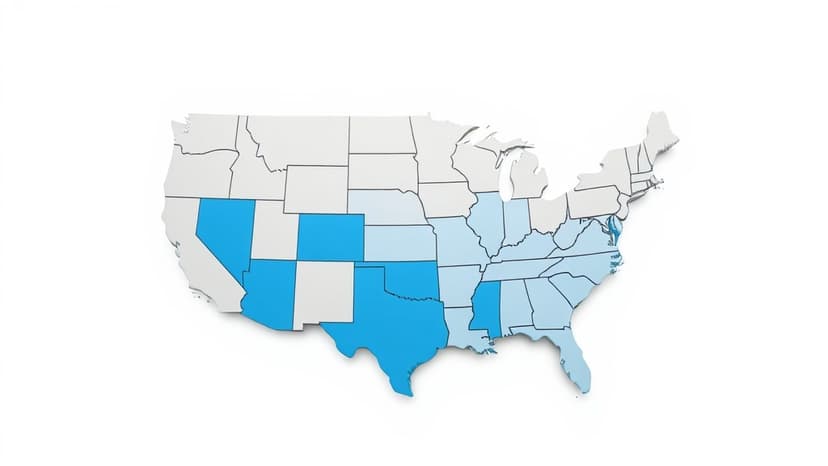
Starting January 1, a new AI-driven pilot program will be implemented in six states: Washington, Arizona, Ohio, Oklahoma, New Jersey, and Texas. This initiative introduces AI prior authorization for traditional Medicare recipients, a process previously uncommon for this segment of beneficiaries. The program's stated goal is to curb fraud and waste by identifying and denying "low-value services."
Despite its objectives, the program has drawn sharp criticism. Experts warn that because AI companies are compensated based on denied claims, the systems are likely programmed to reject more applications. This financial incentive structure raises concerns about increased claim denials, potentially delaying or preventing necessary treatments and impacting seniors' health and finances.
While supporters, including CMS Administrator Dr. Mehmet Oz, believe the AI will streamline processes and reduce abuse, opponents predict it will normalize profit-driven gatekeeping within Medicare. The six-year pilot aims to test these AI systems, with potential nationwide expansion if deemed successful, raising alarms about long-term access to care for millions.



