Home / Health / Thrush Fights Back: Antifungal Resistance Soars
Thrush Fights Back: Antifungal Resistance Soars
1 Dec
Summary
- Candida fungi are developing resistance to common antifungal drugs.
- About 7% of Candida blood samples in the US are resistant to fluconazole.
- Environmental changes and drug overuse fuel the rise of resistant strains.
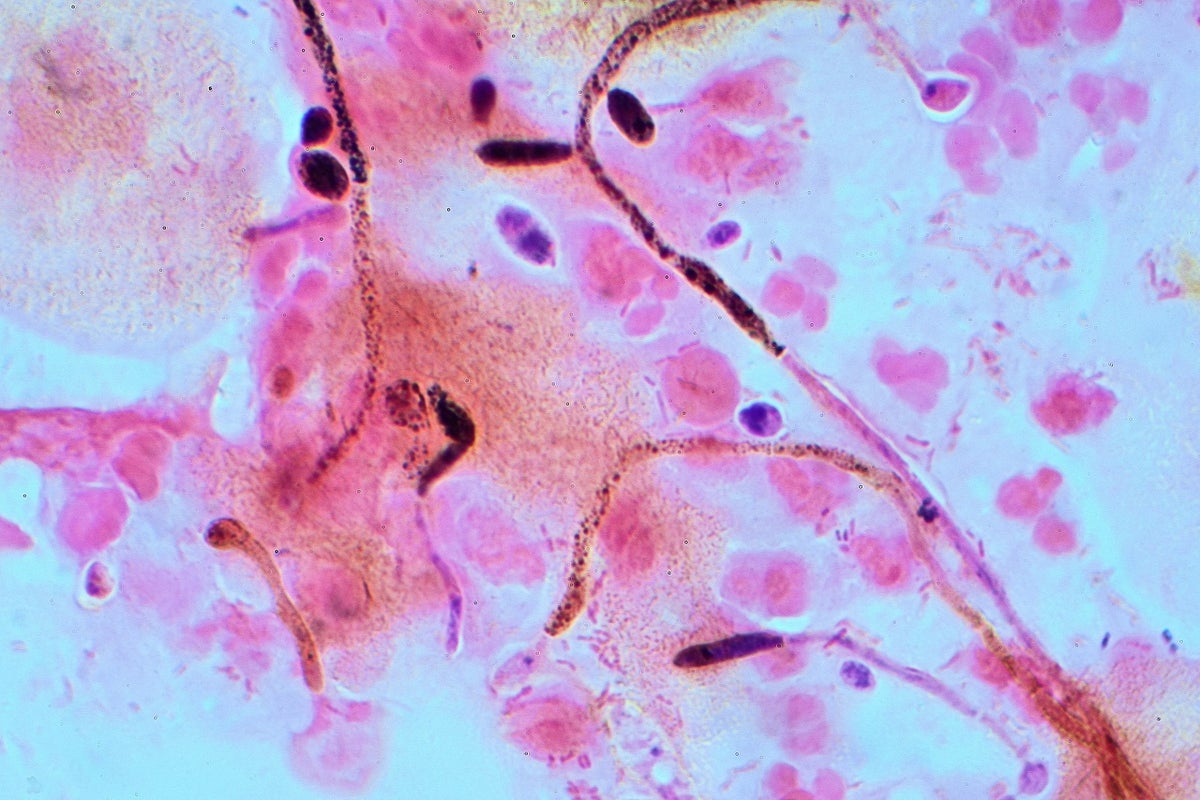
Thrush infections, caused by the Candida fungi, are increasingly difficult to manage due to growing antifungal resistance. Globally, Candida species are adapting, with resistance to fluconazole, a first-line drug, now affecting about 7% of bloodstream infections in the United States. This trend poses a significant challenge, as it limits treatment options for both common thrush and more severe infections, especially in immunocompromised individuals.
The rise in drug-resistant Candida is attributed to several factors. Overuse and misuse of antifungal medications in both human and agricultural sectors, coupled with a limited pipeline of new effective drugs, are primary drivers. Additionally, environmental factors like increasing temperatures and ecological stress are creating conditions that favor the proliferation of resilient strains, such as Candida auris, which is resistant to multiple antifungal classes.
While healthy individuals with robust immune systems are generally protected, disruptions to the body's natural microbiome can allow Candida to overgrow. Taking antibiotics judiciously, maintaining a diverse, fiber-rich diet, and completing full courses of prescribed antifungals are vital steps in preventing the development and spread of resistant strains. Research into new transmission routes, like airborne Candida detected in urban air samples, highlights the evolving nature of this public health concern.



