Home / Health / Aetna Fertility Coverage Lawsuit Settled
Aetna Fertility Coverage Lawsuit Settled
23 Dec, 2025
Summary
- Aetna will now nationally cover fertility treatments for same-sex couples.
- The settlement requires Aetna to pay at least $2 million in damages.
- A California law expands fertility benefits to same-sex couples and singles.
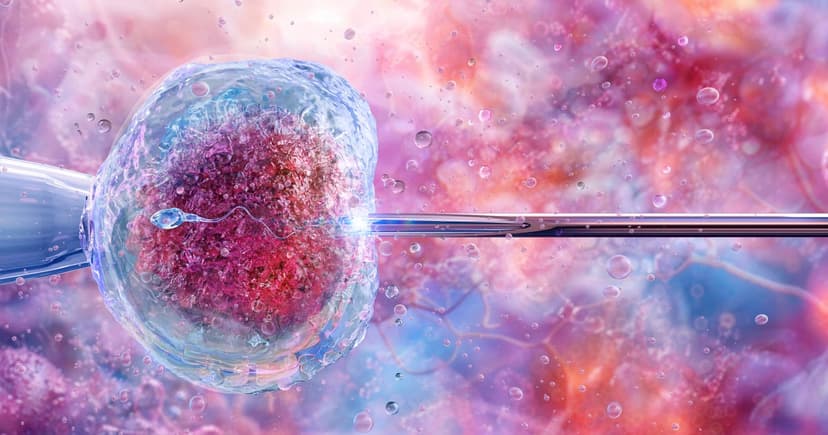
In a significant legal victory, Aetna has agreed to a preliminary settlement requiring them to cover fertility treatments, such as IVF, for same-sex couples nationwide. This agreement, approved by a U.S. District Judge in California, marks the first time a health insurer has been mandated to extend these benefits nationally to LGBTQ+ members. This change rectifies a policy that previously excluded same-sex couples from insurance-covered fertility services, forcing them to pay substantial out-of-pocket expenses.
The settlement also includes at least $2 million in damages for eligible California Aetna members, who must submit claims by June 29, 2026. Previously, Aetna's policy required heterosexual couples to attempt conception for six to 12 months before qualifying for benefits, a condition designed around heterosexual intercourse. This effectively denied coverage to same-sex couples and single individuals, who were often required to undergo numerous artificial insemination cycles before IVF eligibility.
This national settlement coincides with a new California law, effective January 2026, that expands mandated fertility benefits to include same-sex couples and single individuals under state-regulated plans. Experts highlight this as a crucial step toward achieving equity in family-building healthcare, ensuring that all individuals have equal access to reproductive health services regardless of their sexual orientation or marital status.




